Several patient factors should also be considered when choosing between surgery or IVF, including:
- Age
- Ovarian reserve (the number of eggs the patient has)
- Prior fertility outcomes
- Number of children desired
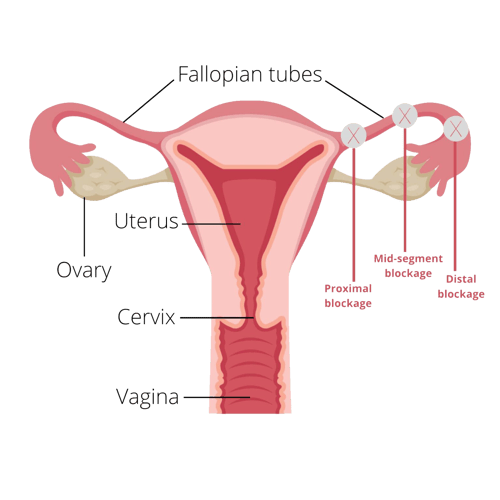
- Site and extent of tubal damage including whether a hydrosalpinx is present
- Presence of other infertility factors
Patient preference, religious beliefs, cost, and insurance reimbursement also figure into the equation. A semen analysis should be performed early in the infertility investigation, as these results may influence the decision between tubal surgery and IVF.
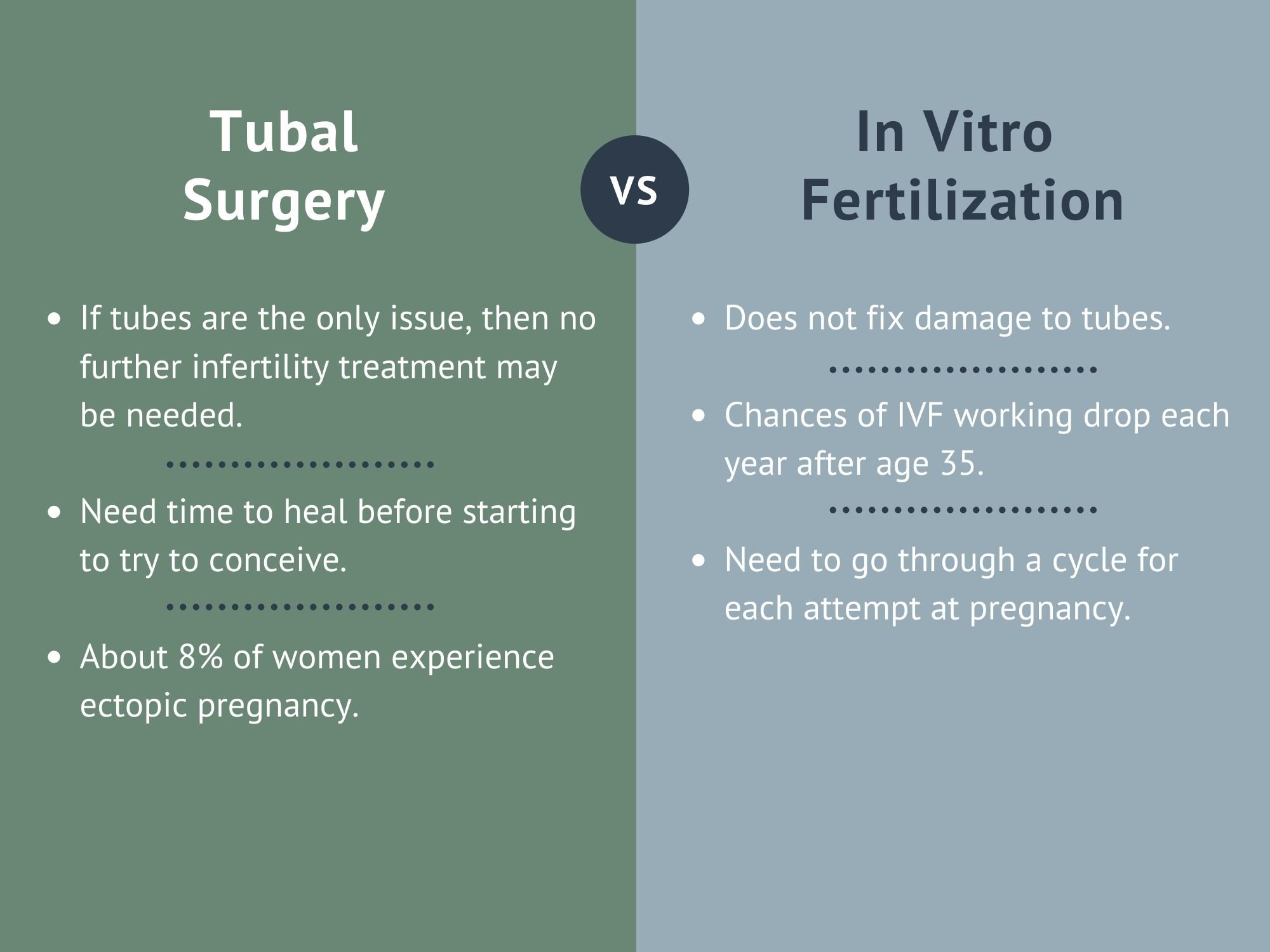
Patients opting for tubal surgery should know that these procedures increase the risk of scar tissue and adhesions. There is also a chance of recurrent blocked tubes after surgery, pelvic infection, or an ectopic pregnancy. The chance of conceiving naturally after surgery is greater if the patient is young and has a minimal amount of scar tissue blocking the fallopian tubes.
The most significant risks of IVF as a tubal treatment include the occurrence of multiples in pregnancy (twins or more, which carries risks for mother and babies) and ovarian hyperstimulation syndrome. This condition occurs when patients over-respond to fertility injections, which can lead to swelling of the ovaries and other severe symptoms including abdominal pain, vomiting, and shortness of breath. Overall, IVF is a very safe and effective fertility treatment for tubal infertility.