 A Day in the Life of Your Fertility Doctor"
class="bg-img"
fetchpriority="high"
loading="eager"
decoding="async">
A Day in the Life of Your Fertility Doctor"
class="bg-img"
fetchpriority="high"
loading="eager"
decoding="async">
Written By: Women & Infants Fertility Center on March 15, 2017
I chose to be a fertility doctor because I love to help people achieve their dream of building a family or preserve their option to do so sometime down the road. But what does this kind of work really look like? Smartphone camera in hand, I set out to give you a glimpse of an average day in the life of your fertility doctor.
A typical day for me starts with a cup of coffee and some quiet time in my office. This is when I like to prepare for the day by reviewing the charts of all the patients on my schedule. One of my key objectives is to ensure that my patients receive care that aligns with their specific goals.
That’s why I maintain a thorough knowledge of their medical history, test results and previous treatment outcomes. Before we meet together face to face, I want to have a good grasp on the details of their situation.

Here's a shot of me performing an egg retrieval.
Today is Friday, and Friday is my favorite day because it’s my day to cover procedures. These include egg retrievals and embryo transfers for patients undergoing in vitro fertilization (IVF), as well as hysteroscopy, where we look inside the uterus with a camera. Unfortunately, these procedure days also sometimes include taking care of miscarriages.
I head up to the fifth floor to meet with my first patient of the day, here for her IVF retrieval. We’re removing her eggs to be fertilized by her partner’s sperm in our IVF laboratory.
In this case, the resulting embryos will be monitored and around day 5 of development tested for chromosome abnormalities that can cause pregnancy failure and birth defects. We can then choose an embryo with the normal number of chromosomes to transfer back into the patient’s uterus at a later date, giving that patient the best chance of a successful pregnancy.
It’s a routine morning up here for a fertility doctor: We have two IVF retrievals, a hysteroscopy and then three embryo transfers. I particularly enjoy the embryo transfers because it is such an important milestone, full of excitement and anxiety for the patients who have worked so hard to reach that!
Now comes the hard part for the patient (and me)…waiting two weeks for the pregnancy test to see if the embryo transfer was successful.
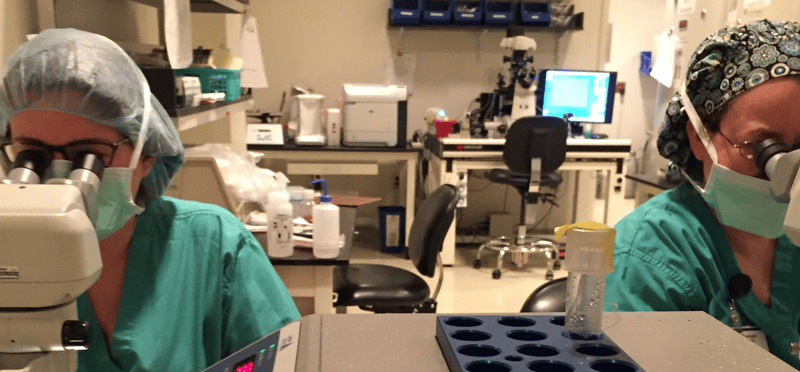
 As I pass the IVF lab, I snap a shot of two embryologists hard at work looking for oocytes after an egg retrieval.
As I pass the IVF lab, I snap a shot of two embryologists hard at work looking for oocytes after an egg retrieval.
I head back down to my office where I eat lunch at my desk. During this time, I usually review the ultrasounds from the morning for all of my patients who are undergoing IVF and intrauterine insemination (IUI) cycles.
The ultrasound is an important tool in the fertility doctor’s diagnostic toolbox. It’s a noninvasive, painless imaging device that allows us to keep a close watch on a woman’s uterus and ovaries, including the follicles being made by her ovaries. This gives us the ability to optimize the timing of egg retrieval, embryo transfer and insemination.
As I munch on my lunch, I’m also looking at blood test results from these same patients. This testing allows us to carefully monitor how our patients are responding to the medications we are administering.
We want to ensure that they’re receiving the perfect dose, and we also want to avoid overstimulation, which can cause complications. After a careful review of their numbers, I make a plan that evening for their medication doses and when they should return for their next ultrasound.
It’s time for my afternoon clinic. Today I am starting off with a new patient, who is here to discuss options for fertility preservation - in her case, freezing eggs to protect her fertility until she finds a partner and is ready to start a family in the future.
Fertility preservation is one of the things I’m most passionate about in my work as a fertility doctor. I love that we have cutting-edge technologies that allow patients the freedom to preserve their reproductive options, be it for personal reasons or for health reasons, such as those banking their eggs or sperm prior to cancer treatment.
Next, I run over to the ultrasound suite to perform a saline sonohysterogram for a patient undergoing a workup to understand the cause of her infertility. For this type of ultrasound, we inject a small amount of saline into the uterus so that we can get a clear picture of the uterine cavity.
After that, I sit down with a returning patient who has done three cycles of Clomid (an oral medication that helps women ovulate) and IUIs, but hasn't yet gotten pregnant. She’s here to discuss next steps.
These can be tough conversations, often going beyond simply discussing clinical details. A lot of emotions accompany failed treatments, and it’s important for me to be available to patients who are feeling discouraged. I try to remind them that fertility treatment is a process – a marathon and not a sprint – and that in almost every case, there is reason to be hopeful and optimistic.
As I say goodbye to my last patient, I return to my office to tie up any loose ends before the weekend. I return phone calls from patients who have called throughout the day with concerns. And then I review any labs that have resulted throughout the day and communicate next steps for patients with my nursing team.
Before I head home I look at the Saturday schedule, since I am on call this weekend. Eggs aren’t only ready for retrieval or embryos prime for implantation 9-5 during weekdays. Then I head home to rest up, since I'll be back at 7 a.m. for more IVF egg retrievals!
There’s always more work to be done and more patients to treat, but to be honest, I can’t think of a more rewarding profession than being a fertility doctor and getting to help people achieve their family building dreams.
Disclaimer: The content in this blog is for informational and educational purposes only and should not serve as medical advice, consultation, or diagnosis. If you have a medical concern, please consult your healthcare provider or seek immediate medical treatment.
Send Us A Message
90 Plain Street,
Providence, RI 02903
Copyright © 2026 Care New England Health System